Vascular Neurology Fellowship

Dr. Davis is the Director of the Vascular Neurology Fellowship, Director of the Harborview Medical Center Comprehensive Stroke Center, and an Associate Professor in the Department of Neurology
The Vascular Neurology Fellowship is one-year ACGME approved program. There are four positions each year. Clinical training is based at Harborview Medical Center, a dynamic county hospital that is also a Joint Commission certified Comprehensive Stroke Center and level 1 Trauma Center caring for approximately 800 ischemic and hemorrhagic stroke patients each year. In addition to the intensive vascular neurology training offered, there are rotations in neuroradiology, neurosoncology and neurocritical care. Call is taken with the acute stroke interventional team and includes video telestroke. There are numerous opportunities to participate in research and fellows are encouraged with faculty support to submit abstracts to the International Stroke Conference. At the end of one year of training, the trainee will be eligible to sit for the Vascular Neurology subspecialty board certification examination. Those trainees interested in research or an academic career will be encouraged to apply for external (AAN, ASA, NIH) research fellowship funding.
Applications are open for the 2026-2027 Fellowship
Pediatric Vascular Neurology Track
Starting with academic year 2024-2025 we are offering a dedicated slot for a Child Neurology applicant to pursue a Pediatric Vascular Neurology fellowship with ACGME accreditation. The Pediatric Track will offer additional clinical and research time at Seattle Children’s Hospital and mentorship from Dr. Amlie-Lefond, a national leader in Pediatric neurovascular disease. The Vascular Neurology program at Seattle Children’s Hospital, established in 2011, is a leading multidisciplinary program in the Pacific Northwest, catering to children with neurovascular disorders.
The addition of a Pediatric Vascular Neurology track enhances the current Adult Vascular Neurology training by broadening the scope of the fellowship and offering our adult fellows more interaction and comfort with the field of Pediatric Vascular Neurology.
Why UW Vascular Neurology?

We have a unique geographic location – as the only academic medical center in the Seattle metropolitan area and because we draw patients from a broader region, including Alaska, our patient population is rich and offers a wealth of learning.



Our faculty are smart, accessible, and remarkably approachable. Anyone at almost any time is happy to sit down and discuss a patient issue or personal concern.

Seattle is a phenomenal place to live! Not only do we have a thriving city with great food and cultural activities, but we have easy access to water and mountains as well. Where else can you see sea lions and a volcano (Mt. Rainier) on your commute to work each day?
Vascular Neurology Rotations
Inpatient Stroke
Spend time rounding with the inpatient teams at Harborview Medical Center learning from the vascular neurology faculty, neurocritical care faculty, sharing your expertise with trainees, responding to stroke codes, and helping to guide the care of stoke patients admitted to a comprehensive stroke center.
Inpatient rounds include daily rounds in the neurocritical care unit where we co-manage patients with the most severe strokes.
Stroke Phone
Take shifts triaging and answering consult questions from providers at UW Medicine hospitals and partners throughout the WWAMI region including critical access hospitals in rural and underserved areas. In addition to strengthening your vascular neurology knowledge, you will gain skill in conducting patient evaluations via TeleStroke and learn how to appropriately triage patients across a large geographic area based upon need and availability of resources. Night and weekend shifts on the stroke phone are done from home.
Neurocritical Care Service
You will spend time caring for patients with severe stroke including subarachnoid hemorrhage, traumatic brain injury, and other severe neurological injury in the neuro ICU at Harborview Medical Center, learning from neurocritical care specialists with a variety of backgrounds including neurology, neurosurgery, neurointerventional, and anesthesiology. Differs from the inpatient rotation in that you will also see the patients co-managed with the neurosurgery service (subarachnoid hemorrhage, traumatic brain injury and spinal cord injury)
Transcranial Doppler Rotation
Learn the basics of performing and interpreting transcranial doppler ultrasound imaging by working closely with the Harborview Cerebrovascular Lab. For those who would like to pursue certification in TCD interpretation you will have the opportunity to complete the required number of studies to sit for the exam.
Neuroradiology
Work side by side with the neuroradiology fellows and attendings to deepen your knowledge and ability to interpret neuroimaging. You will also spend time observing neurointerventional cases and will have designated self-study time with suggested learning resources.
Research Elective
This time is designed to help you develop new projects or get ongoing projects across the finish line. Our faculty have a number of research and quality improvement projects that fellows can participate in. We are also happy to support the development of new projects.
Other Electives
Fellows may opt to spend additional time on any of the above. Other popular options include Palliative care, Rehabilitation, Neurology consults, Neuro-intervention. Generally we are happy to work with you to arrange electives of interest!
Stroke Clinic
Fellows have the opportunity to care for outpatient vascular neurology patients in half-day clinics each week. The clinic is staffed by vascular neurology attendings and provides an opportunity for continuity of care and for managing chronic neurovascular conditions such as moya-moya syndrome and CADASIL. In addition, fellows have the unique opportunity to spend some time in clinic at Seattle Children’s Hospital under the mentorship of our pediatric vascular neurology expert, Dr. Amlie-Lefond.

Conferences
- Monday stroke webinar (topics from the prior year include International Stroke Conference, NIH Stroke Net Grand Rounds, World Stroke Organization, and more).
- Wednesday noon Neurology Lecture Series (including a monthly stroke lecture and visiting stroke faculty annual lecture)
- Thursday afternoon Neurology Grand Rounds
- Friday afternoon stroke didactics followed by a multi-disciplinary stroke clinical conference (discussion of interventions and challenging or interesting cases of the week)
In addition, fellows are encouraged to attend the International Stroke Conference as well as other national conferences, especially if presenting research.
Teaching opportunities for fellows abound – fellows participate in the Neurology Lecture Series and lead various medical student and resident didactics throughout the year.
How to Apply
Our program participates in the NRMP Match using ERAS for Fellowship Positions. Please upload your C.V., 3 letters of recommendation including a letter from your current program director, a personal statement, and your USMLE Scores into the ERAS program. Applications will be reviewed starting December and interviews will follow.
Prior to appointment in the program, fellows must have successfully completed an ACGME-accredited program in neurology, child neurology, neurodevelopment disabilities, or a program in one of these specialties that is located in Canada and accredited by the Royal College of Physicians and Surgeons of Canada.
To Apply
All applications are submitted through the Electronic Residency Applicator Service (ERAS). Information regarding ERAS can be found on National Residency Matching Program (NRMP). Interviews will be conducted in early 2025
For any questions or to submit additional materials for your application please contact our Program Coordinator, at neurofellowship@uw.edu.
Core Fellowship Team

Catherine Amlie-Lefond, M.D.
Dr. Amlie-Lefond is the Director of the Pediatric Vascular Neurology program at Seattle Children’s Hospital and a Professor of Neurology. She is the site director for the fellowship at Children’s and helps direct the Pediatric Vascular Neurology track.
Special Clinical and/or Research Interests:
Pediatric stroke, acute treatment of stroke, cerebrovasculopathy and cerebral vascular malformations

Claire Creutzfeldt, M.D.
Dr. Creutzfeldt is a vascular neurologist at Harborview, the Director of Neuropalliative Care, and an Associate Professor of Neurology.
Special Clinical and/or Research Interests:
Neuro-palliative care, especially for patients with severe acute brain injury.

Rizwan Kalani, M.D.
Dr. Kalani is an Assistant Professor of Neurology.
Special Clinical and/or Research Interests:
Lipids and cerebrovascular disease, stroke epidemiology and population-based approaches to stroke prevention in low-and middle-income countries.

Ryan Kiser, M.D.
Dr. Kiser is an Assistant Professor of Neurology.

Sandeep Khot, M.D., M.P.H.
Dr. Khot is the Director of the HMC Consult Service and a Professor of Neurology.
Research Interests:
Dr. Khot conducts clinical research on the relationship between sleep apnea and stroke, notably assessing stroke recovery with the treatment of sleep apnea with continuous positive airway pressure (CPAP). Other research includes cardiac arrest, carotid dissection, intracranial atherosclerosis, giant cell arteritis, and stroke.
Clinical Interests:
Care of hospitalized patients with neurologic disease.

Will Longstreth, M.D.
Dr. Longstreth is the chief of Neurology at Harborview Medical Center, Professor of Neurology, and an Adjunct Professor of General Internal Medicine, Epidemiology, and Medicine.
Clinical and/or Research Interests:
Cerebrovascular disease and epidemiology.

Hope Opara, M.D.
Dr. Opara is a Clinical Assistant Professor of Neurology.
Special Clinical and/or Research Interests: Acute stroke intervention and management, primary and secondary stroke prevention, and use of transcranial doppler particularly for surveillance of cerebrovascular disease severity in sickle cell patients.

Breana L. Taylor, M.D.
Dr. Taylor is an Assistant Professor of Neurology. She is the Associate Program Director of the Vascular Neurology Fellowship and Head of the Mt. St. Helens College in the UW School of Medicine.
Special Clinical and/or Research Interests:
Medical education and neuro-palliative care communications education.

David Tirschwell, M.D., M.Sc.
Dr. Tirschwell is the Medical Director of Comprehensive Stroke Care at the UW Medicine Stroke Center at HMC and a Professor of Neurology.
Research Interests:
Intracerebral hemorrhage, stroke epidemiology, quality of care, clinical trials and outcomes of stroke patients.

Natlie Weathered, MD, MS
Dr. Weathered is the Program Director of the Neurology Residency Program and a Clinical Assistant Professor of Neurology.

Jonathan Weinstein, M.D., Ph.D.
Dr. Weinstein is a Professor of Neurology and an Adjunct Associate Professor of Neurological Surgery.
Special Clinical Interests:
CNS Vasculopathies, neurovascular leukoencephalopathies
Special Research Interests:
Basic and translational work on the neuroimmune responses in both acute stroke and in ischemic preconditioning.
Dr. Weinstein’s Research Laboratory: https://neurology.uw.edu/research/weinstein-lab/research.html

Vivian Yang, M.D.
Dr. Yang is an Assistant Professor of Neurology and the course director of the Mind Brain & Behavior Course for the UW School of Dentistry.
Fellows also work extensively with our neuro-interventionalists, neurocritical care, neuroradiology, and neurosonology faculty, among others.
Current Fellows

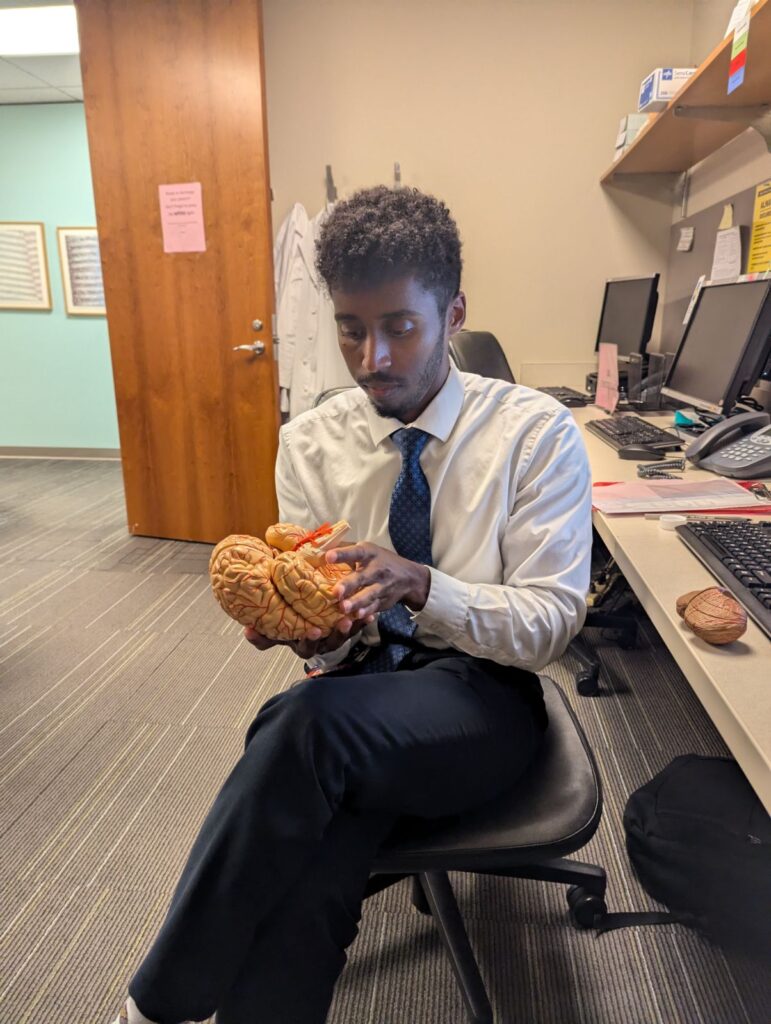
Amen Yonas, MD
Amen was born in Atlanta, Georgia but was raised in Houston, Texas. Prior to medical school he worked as an MCAT and high school/college physics tutor. He earned his medical degree at UT Southwestern in Dallas. TX. Afterwards he completed his neurology residency at Mayo Clinic in Jacksonville, Fl. Within medicine his general interests include medical education and working with underserved populations. His research interests include post stroke epilepsy, and cerebral amyloid angiopathy. Outside of medicine he enjoys reading, weightlifting, running, board games, and chasing his dog Lou.

Lori Xu, MD
Lori grew up all over the States, ending high school in Austin, TX. She completed her B.A. in Biology at Washington University in St Louis before returning to Texas for medical school and Child Neurology residency at UT Southwestern/Children’s Medical Center in Dallas. Her clinical and research interests involve the pediatric neurovascular population and the younger adult population with strokes. Outside of medicine, she relishes live music and concerts, running/other workouts (HIIT, yoga, hiking), traveling.

Natasha Khan, MBBS
Natasha is originally from Pakistan but moved to Oregon for the love of her husband and horses. She completed her medical degree at The Aga Khan university in Karachi, Pakistan and residency at the University of New Mexico, where she was a Chief Resident. Her clinical interests are in education, QI, and learning about health care policies in developing countries. In the vascular realm, she is fascinated with intracerebral hemorrhage and large artery etiologies, mostly cervical artery dissections. Outside of work, she is a mom, a wife, an aspiring endurance rider, an Arabian horse breeder, and she loves mountains.

Gitanjali Das, MD
Gitanjali Das grew up in San Diego, California and went to Ohio State University in Columbus, OH for medical school. She made her way back west to University of Utah for her neurology training, where she was Chief Resident of Education. Her clinical and research interests are in Vascular Neurology, Palliative Care, Improving Access to Care, and Anti-Racism in Neurology. Outside of work, she enjoys baking, cooking, drinking too much coffee, live music, and singing poorly at karaoke.
Fellowship Graduates and Post-Graduate Employment
2023-2024
Kafi Hemphill, M.D. – UCSF NeuroIR fellowship 2024-2026
Meghan Romba, M.D. – Providence Oregon Teleneurology
Shannon Tierney, M.D. – St Luke’s Medical Center, Boise, ID
Farrah Khan, M.D. – Sevaro Teleneurology and Telestroke and part-time at University of Washington/Harborview Medical Center in stroke clinic, Seattle, WA
2022-2023
Matt Murphy, M.D. – University of Colorado Health (Fort Collins, CO)
Amy Steinberg, M.D. – TeleSpecialists and Indian Health Services
Hope Opara, M.D. – University of Washington/Harborview Medical Center
2021-2022
Ryan Kiser, M.D. – University of Washington Harborview Medical Center (Seattle)
Rachel Schutz, M.D. – Evergreen Heath Medical Center
Nandini Abburi, M.D. – Duke Raleigh Hospital
2020-2021
William Lou, M.D. – Swedish Medical Center (Seattle)
Markus Hannan, M.D. – UCHealth at Memorial Hospitals
Amita Singh, M.D. – University of Florida Health
2019-2020
Smita Holden, M.D. – Our Lady of Lourdes (Camden, NJ) and University of Pennsylvania hospitals (Philadelphia, PA)
Carson Van Sanford, M.D. – Providence Everett (Everett, WA)
2018-2019
Breana Taylor, M.D. – University of Washington/Harborview Medical Center
James Wang, M.D. – Swedish Medical Center (Seattle)
2017-2018
Steve O’Donnell, M.D. – Virginia Mason (Seattle)
Jenny Siv, M.D. – Providence Everett (Everett, WA)
Diversity Statement
The UW Neurology Department is committed to recruiting, training and promoting a diverse community of scholars. We welcome diverse individuals and are committed to including residents and faculty of diverse race, ethnicity, gender, and sexual orientation. We believe that diversity and inclusion are crucial components in providing both excellent patient care and an excellent learning environment.