Observation Program
Definition of Observation
Medical observations, often referred to as observations or job shadowing, are opportunities for undergraduate students, senior high school students, or other medical professionals to observe a faculty member in their work. Observers are not permitted to touch patients, regardless of background and training; No patient care or hands-on medical training will be conducted, and they will not have direct contact or unsupervised access to patients.
Observations are designed as:
- An educational tool
- An opportunity to gain insight into the medical field through a firsthand view of clinical practice
- A mentorship opportunity for those pursuing or advancing a career in medicine
There will be no compensation provided by the medical administration. Any costs associated with travel, parking, and accommodations are the responsibility of the observer.
Please note that we are currently unable to accommodate requests for shadowing, observations, or audition electives for International Medical Graduates (IMGs).
Submit your pre-application form
Specialties Available for Observation
- General Neurology – General neurologists diagnose and treat a wide range of neurological disorders that affect the brain, spinal cord, nerves, and muscles. Common conditions include headaches, seizures, neuropathy, dizziness, tremors, and memory problems. They often serve as the first point of contact before referral to subspecialists.
- Child Neurology – Medical specialty focused on diagnosing, treating, and managing disorders of the brain, spinal cord, nerves, and muscles in infants, children, and adolescents. Please note, Child Neurology observations are completed at Seattle Children’s Hospital and therefore have a separate list of requirements and paperwork to complete. In order to participate in a Child Neurology observation, you must be at least a high school graduate.
- Neuro-oncology – Neuro-oncologists specialize in diagnosing and managing cancers that affect the brain, spinal cord, and peripheral nerves. This includes primary tumors (e.g., gliomas, meningiomas) and neurological complications of systemic cancers.
- Neuro-immunology – This subspecialty focuses on autoimmune and inflammatory disorders of the nervous system. Common diseases include multiple sclerosis (MS), neuromyelitis optica spectrum disorder (NMOSD), and autoimmune encephalitis.
- Neurohospitalist – Neurohospitalists are neurologists who provide inpatient care, often managing acute neurological events like strokes, seizures, altered mental status, or complex diagnostic cases. They work closely with hospital teams and may coordinate care transitions and evaluations for patients admitted under other services.
- Neurogenetics – This field focuses on neurological conditions caused by genetic mutations, including inherited disorders like muscular dystrophies, hereditary neuropathies, Huntington’s disease, and mitochondrial disorders. Neurogeneticists often work closely with genetic counselors and use advanced diagnostics like whole exome sequencing.
- Movement Disorders – This specialty addresses conditions that affect the speed, quality, and control of voluntary movement. Common examples include Parkinson’s disease, dystonia, essential tremor, Huntington’s disease, and tic disorders.
- Adult or Pediatric Epilepsy – Epileptologists specialize in diagnosing and treating seizure disorders in both adults and children. They interpret EEGs, manage anti-seizure medications, and evaluate surgical options for refractory epilepsy. Pediatric epilepsy specialists focus on early-onset syndromes and developmental epileptic encephalopathies.
- Vascular Neurology/Stroke Care – Vascular neurologists diagnose and treat conditions related to blood flow in the brain and spinal cord, most commonly ischemic and hemorrhagic strokes. They are often involved in acute stroke treatment (e.g., tPA, thrombectomy) and secondary stroke prevention.
Locations Available
- University of Washington Medical Center (UWMC)
- Out-patient only
- Harborview Medical Center (HMC)
- In-patient and out-patient
- University of Washington Medical Center – Northwest
- In-patient and out-patient
Requirements for Observation
To participate, you must:
- Provide valid state or federal photo identification.
- Be a college/university undergraduate student, senior high school student, or healthcare professional in good standing
- Submit up-to-date immunization records from your primary care provider’s office stating the required immunizations listed in the application forms.
Process for Requesting an Observation
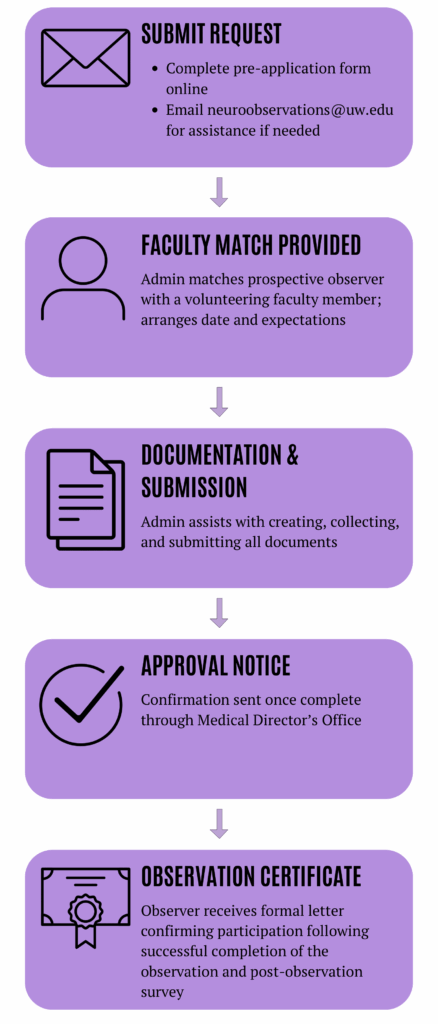
*Please email neuroobservations@uw.edu if you have any questions or concerns regarding observations.
Submit your pre-application form
Frequently Asked Questions (FAQs)
1. Do I need a flu vaccination?
If your observation is scheduled to take place between October 1st and March 31st, you are required to provide documentation of a current flu vaccination for that year. This ensures the safety of both patients and staff during flu season.
2. What works for vaccination proof?
Acceptable proof includes clear images or PDF files of official vaccination records issued by a medical clinic, pharmacy, or healthcare provider. Records must clearly show your name, the type of vaccine received, and the date(s) it was administered.
3. What forms of identification are accepted?
A valid, unexpired state or federal photo ID is required. This includes a driver’s license, state-issued ID card, or passport. School IDs and other unofficial forms of identification are not accepted.
4. How many days can I observe?
Observations are limited to three full days or six half-days per calendar year, depending on availability and faculty schedules..
5. I am 16, can I observe?
High school seniors and individuals under 18 may be considered for observation opportunities on a situational basis depending on availability and faculty approval. They are not permitted in operating rooms.
6. What if I want to observe other groups outside of Neurology?
You will need to contact each department individually.
7. How do I obtain my temporary badge?
After you have been approved to observe, you will receive instructions on how and when to pick up your temporary badge.
8. What does a typical day of observation look like?
This will vary depending on whether you are observing in an inpatient or outpatient setting, as well as the physician’s clinic schedule. You will work out the specifics of hours and days directly with your faculty member. As an observer, you will not be permitted to touch patients. The physician will always ask the patient’s permission before you enter the room, and only if the patient agrees will the visit proceed. Every day is different, but the goal is to give you an authentic view of clinical practice in neurology.
9. What should I bring on the day of my observation?
Faculty members typically share specific instructions once you are matched with them, such as where to meet, what time to arrive, and any additional items they recommend bringing. Please be sure to review these details carefully before your scheduled observation. General guidance on professional dress is also included below.
10. How can I give feedback on my observation?
Click here or email neuroobservations@uw.edu.
Standards of Dress and Appearance in Clinical Settings
Dress and appearance standards are designed to ensure that students present a professional appearance consistent with what is expected in a clinical setting. How one looks and acts directly affects how the care provided is perceived by patients, faculty, staff, and other students.
- Clothing: Clothing should be neat and clean and appropriate for the clinical setting. Items that are not appropriate in the patient care setting include: blue jeans, tank tops, sleeveless shirts, low cut necklines, shorts; overalls; sweats; exposed backs or midriffs or any revealing clothing that exposes undergarments; skirts shorter than 2-3” above the knee.
- Shoes: Closed-toe shoes must be worn in all patient care areas, per OSHA regulations. Flip-flops, slippers, or open-toed shoes/sandals are not allowed in patient-care settings.
- Hair: Hair must be neatly groomed and clean. Long hair must neither obstruct vision nor interfere in any way with the student’s performance. A hair restraint, i.e., hair net, may be required in certain settings. Also, hair color and style must be appropriate for the clinical work environment.
- Facial hair: Facial hair must be neatly groomed, clean, and must not interfere in any way with the student’s performance. For safety and infection control reasons, students working in some areas of the hospital, such as operating rooms, may not be permitted to wear beards, or may be required to wear beard guards.
- Jewelry: Jewelry worn by students must be of reasonable shape and size, appropriate to the work setting, and may not interfere with patient care or safety. Earrings and small nose studs are the only acceptable forms of visible pierced jewelry. Rings must be small enough to allow for the use of gloves, with no risk of tearing the gloves.
- Tattoos: If a tattoo could be interpreted as being obscene, indecent, extremist, racist, or sexist, it should be covered.